
Wasting & Stunting
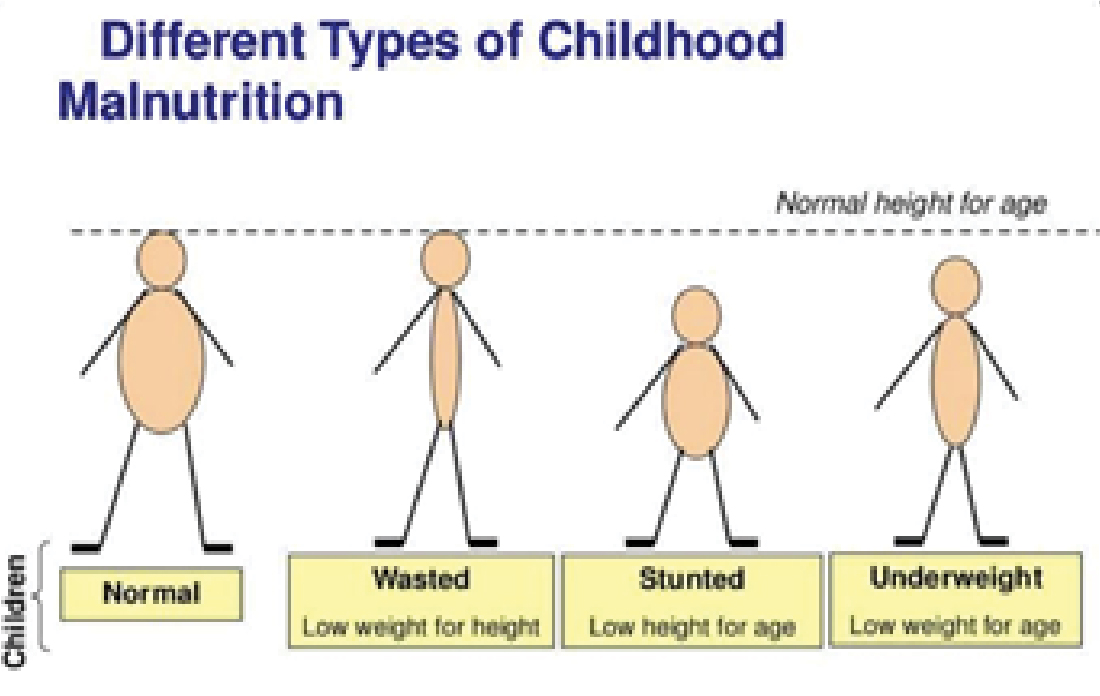
Indonesia experienced an important event in becoming a middle-income country. These include reducing child mortality rates and increasing children's enrollment in elementary schools. However, there has been no improvement in children's nutritional status. There are still many children and teenagers threatened by the high number of children who are thin (wasting) and short (stunting)¹.
Thin Body (Wasting)
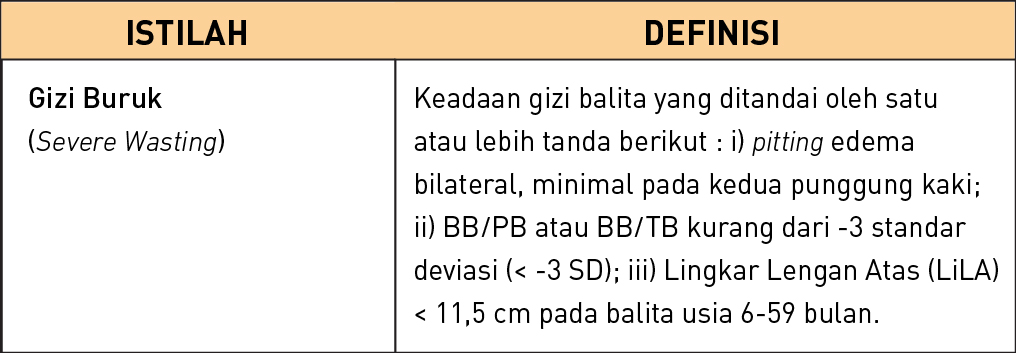
Thin children are the condition of children suffering from nutritional disorders with the diagnosis made through assessment of body weight (BB) and height (TB). Wasting is a condition of acute malnutrition, the child's weight does not match TB or the Z-score value is less than -2SD (Standard Deviation). Thin children are a nutritional problem due to events that occur in a short time such as lack of food intake. If the Z-score measurement is less than -3SD it is called very thin (Severely Wasting) or Malnutrition².
2018 Basic Health Research data shows the prevalence of wasting in toddlers is 10.2% and 3.5% (around 805,000) of toddlers are severely wasting. Based on the map of the percentage of very thin and underweight aged 0-59 months by province in 2016, none of the 34 provinces are free from acute nutritional problems, because the prevalence of acute nutrition in all provinces in Indonesia is > 5% (WHO standard)³
There are 3 categories of causes of wasting, namely maternal factors (exclusive breastfeeding, parenting style, level of education, level of knowledge), child factors (gender, age, nutritional intake, infectious diseases and LBW), family factors (family food security, economic level and number of members). Family)² ³.
Prevention of Malnutrition
Prevention of malnutrition for toddlers needs to be done as early as possible, following general principles and according to the age of toddlers¹.
› Preparations for the health and nutritional status of pregnant women are carried out
since adolescence and during childbearing age
• Implement a healthy, balanced nutritional lifestyle for
meet nutritional needs and prevent
Chronic Energy Deficiency (KEK).
• Consume Blood Supplement Tablets (TTD).
• Get premarital counseling.
• Prevent early marriage and teenage pregnancy.
• Increase participation in Family Planning (KB).
• Implement personal hygiene and sanitation practices
as well as the environment.
› Pregnant women receive Antenatal Care (ANC) services
integrated quality according to standards.
› Improved nutritional and health status, growth and development
and child survival through strategy
Infant and Child Feeding (IYCF) is carried out using the "Gold Standard of Infant and Child Food" practices.
• Early Initiation of Breastfeeding (IMD)
• Exclusive breastfeeding (0-6 Months)
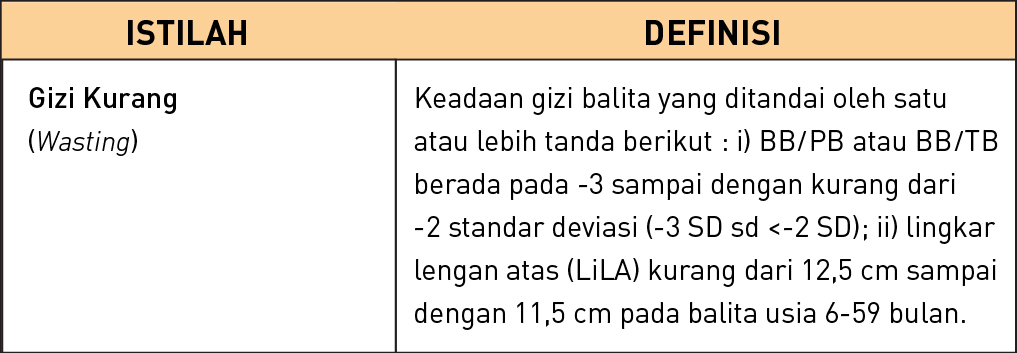
• Providing MP ASI starting at 6 months of age
• Continue breastfeeding until the age of 2 years or more
Phase of Care and Treatment of Malnutrition in Toddlers
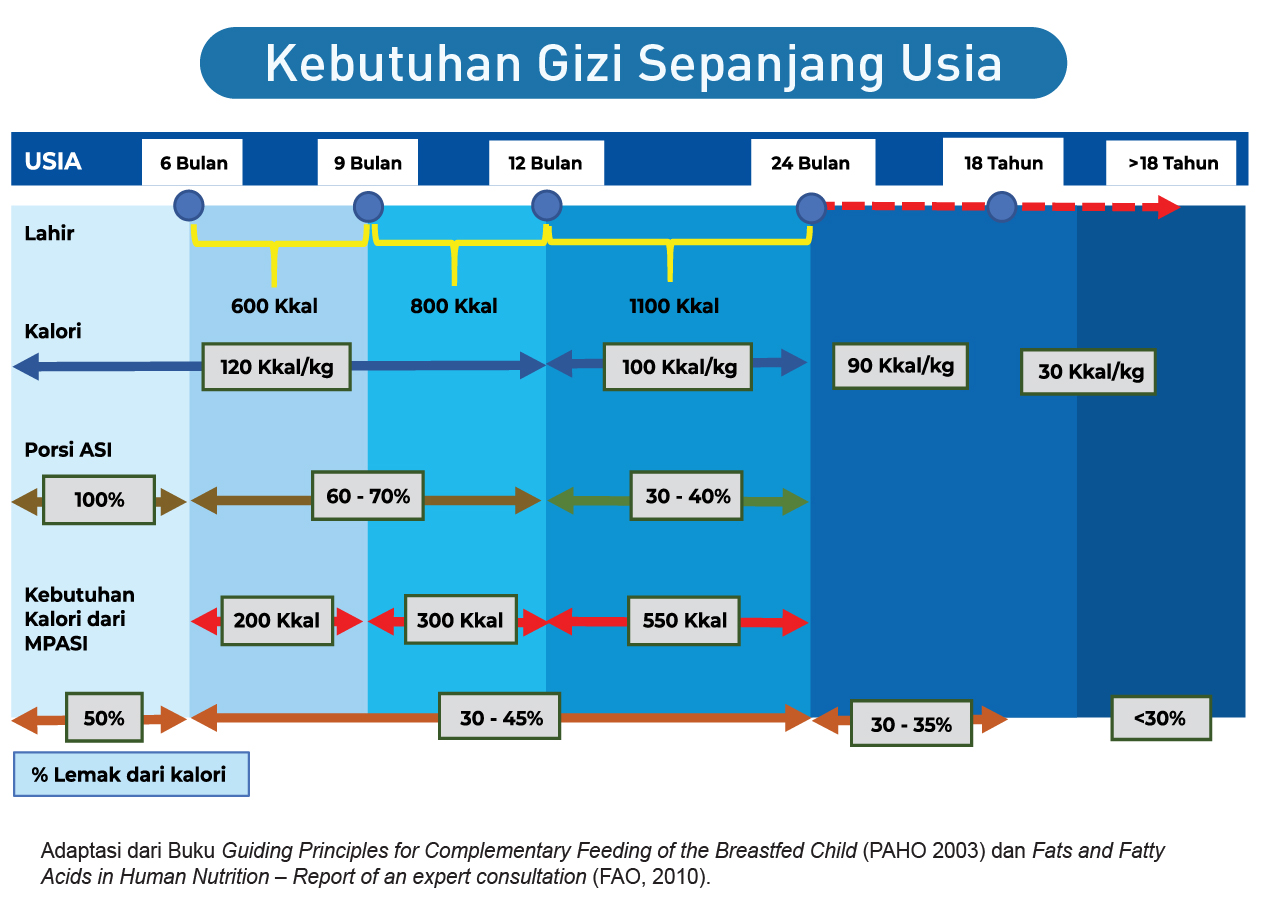
1. Stabilization Phase: the initial phase of treatment is generally 1-2 days, but can continue for up to a week according to the child's clinical condition. This monitoring phase records vital signs (pulse, respiratory rate, body temperature), danger signs, degree of edema, formula intake, frequency of defecation, stool consistency, urine volume and body weight.
2. Transition Phase: the transition period from the stabilization phase to the rehabilitation phase, the aim of which is to give the body the opportunity to adapt to the increased supply of energy and protein. This monitoring phase is like the stabilization phase.
3. Rehabilitation Phase: this phase is provided in outpatient and inpatient services, the phase of providing food for catch-up growth. Providing energy of 150-220 kcal/kgBB/day in the form of F100 or RUTF, gradually adding food according to body weight, for 2-4 weeks. Therapeutic progress was assessed by weight gain after the transition phase and receiving F100 or RUTF.
4. Follow-up Phase: continued provision of food for catch-up growth with family feeding and Recovery Supplemental Feeding (PMT-P)¹.
Short Stature Children (Stunting)
Stunting is a condition of malnutrition related to past nutritional deficiencies, including chronic nutritional problems. Stunting is measured as nutritional status by taking into account the height or length, age and gender of the toddler. Stunting or short stature (shortness). In a situation where height (TB) does not match age, the determination is made by calculating the Z-score for height according to age (TB/U). It is said to be stunting if the TB/U Z-score is below -2 SD (Standard Deviation).
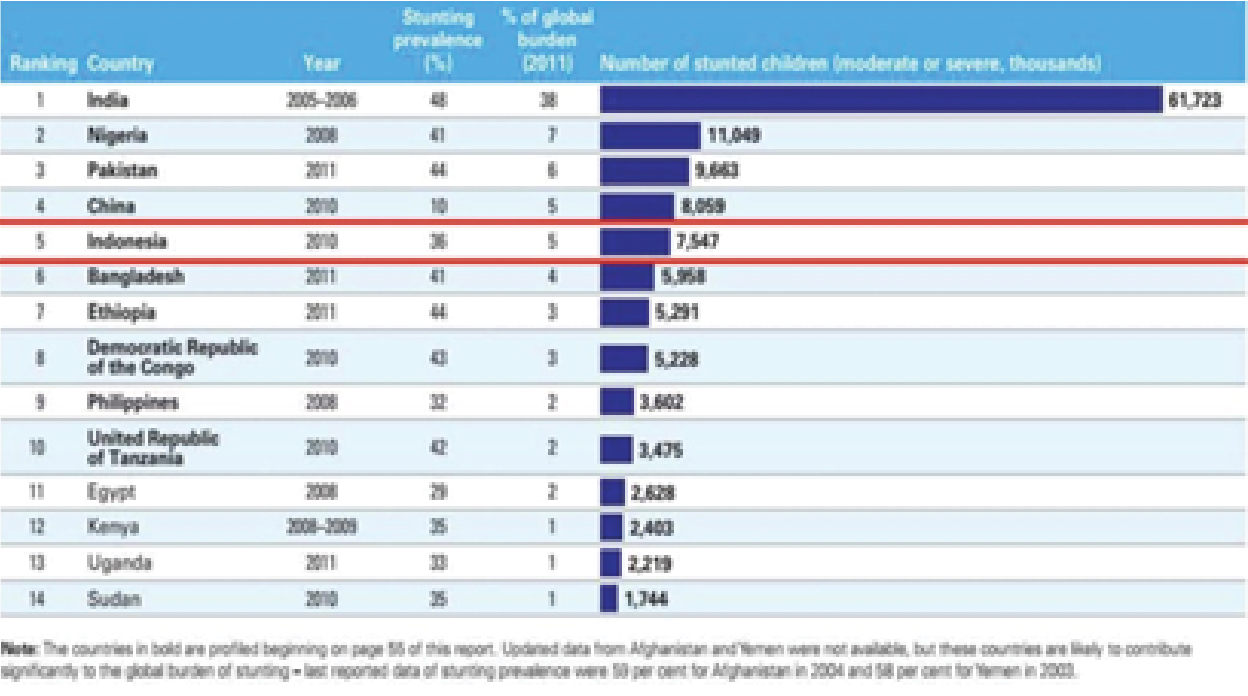
Stunting is caused by multi-dimensional factors, not only poor nutrition experienced by pregnant women and children under five. Interventions to reduce the prevalence of stunting are carried out in the First 1000 Days of Life (HPK) of children under five. 1000 HPK consists of 270 days during pregnancy and 730 days (two years) of the child's life. Several factors that cause stunting are as follows:
• Poor parenting practices, lack of maternal knowledge regarding health and nutrition before and during pregnancy and after the mother gives birth.
• Limited health services including ANC-Ante Natal Care (health services for mothers during pregnancy), Post Natal Care and quality early learning.
• Lack of household access to nutritious food, because it is expensive in Indonesia.
• Lack of access to clean water and sanitation.
Another factor is Chronic Energy Deficiency (CED) in women aged 15-49 years, whether pregnant or not pregnant. According to Riskesdas 2013, the prevalence of CED risk in pregnant women is 24.2%, in non-pregnant women it is 20.8%.
Strategy to Overcome Stunting
Referring to UNICEF/Lancet, stunting is caused by the influence of parenting patterns, coverage and quality of health services, the environment and food security. Parenting patterns and family level food security are linked to the program implementation strategies that must be implemented. Caring patterns, including Early Breastfeeding Initiation (IMD), exclusive breastfeeding (ASI) for up to 6 months, followed by Complementary Feeding for Breast Milk (MPASI) for up to 2 years to help the growth and development of babies and children. The low IMD and exclusive breastfeeding concerns breastfeeding counselors who are not evenly distributed in all health centers.
Breastfeeding counselor training is carried out at the district level, but there is no information about the percentage for all Community Health Centers. The Community Health Center does not yet know what percentage of counseling staff the importance of IMD and exclusive breastfeeding. Another gap is still weak monitoring of violations and law enforcement regarding the use of formula milk and not all workplaces provide breastfeeding areas as needed.
Babies over 6 months old, even though they are still breastfeeding for up to 2 years, need complementary foods to fulfill nutritional requirements for growth. WHO/UNICEF requires that babies aged 6-23 months receive adequate MPASI provided they can receive at least 4 or more of 7 types of food (cereals/tubers, nuts, dairy products, eggs, other sources of protein, rich vegetables and fruit). vitamin A, vegetables and fruit-Minimum Dietary Diversity/MMD).
In addition, babies must meet the Minimum Meal Frequency (MMF) provisions, namely babies aged 6-23 months who are given or not given breast milk, have received MP-ASI (soft/solid food, including those who do not receive breast milk), the frequency of giving is as follows: following:
› Breastfed babies :
• Age 6-8 months: 2X/day or more
• Age 9-23 months: 3X/day or more
› Babies 6-23 months who are not breastfed: 4X/day or more.
Bibliography
1. RI KK. Prevention and Management of Malnutrition in Toddlers in Outpatient Services.
Medicine 2020.
2. Factors Behind the Incident of Wasting in Children Under Five.
Medicine 2020.
3. Andalas University. Relationship and magnitude of risk factors in underweight children under five from poor families in Solok City.
Medicine 2019.
4. Mayasari D. Stunting, Risk Factors and Prevention. Medicine 2018.
5. Indonesian Ministry of Health. Situation of Short Toddlers (Stunting) in Indonesia. Medicine 2018.
By:

dr. Yohanes Tri Nugroho, MSi., Med., SpA
Pediatrician Specialist at Santo Borromeus Hospital



